I had read the books, painted the nursery, washed and folded the pre-loved newborn clothes and even had my hospital bag packed by the time I read the comments on my 31-week ultrasound report.
I had a non-standard ultrasound due to experiencing some pain and I remember thinking how lucky I was to have another look at my Squishy. The scan went well and I was reassured until the next week, when reading the text at the bottom of the scan report.
Those words suggested something was unexpected about the way Squishy’s brain was growing. Without knowing what this meant, I first asked the doctors I worked with, but they weren’t sure either, so I sought help from Google, which quickly brought up many words that felt scary at the time.
Knowing that Google is not the most reliable, I threw myself into medical journals, although they brought little comfort as they again repeated the odds and outcomes that an internet search offered.
After leaving a message on a fetal medicine clinic message service, I couldn’t do much else but cry. It was a few days before the three-hour long drive from the country to the city and sitting in the dark room for my Level 2 scan. The sonologist confirmed that the scan was correct and there was also another possible finding.
When I asked what happens next, with kindness and empathy I was told that I can be booked into that hospital and undergo a termination of pregnancy and tell friends and family I had a stillbirth. I asked about further tests, as my own reading had suggested a fetal MRI would be recommended, especially with the unknown of the other potential neuroanatomical anomaly too. I was told that the tests were possible, but were “not cost-effective” if I was planning to terminate.
After opting for tests, I joined many other pregnant women in several waiting rooms that day as I waited for an amniocentesis, then waited to speak to three specialists in the afternoon who were going to tell me what the diagnosis was going to mean.
All three specialists, while caring and kind, couldn’t actually tell me what was to come. They spoke of odds and listed off potential syndromes, medical conditions and disabilities, much like Google did and like the journal articles did. Each also raised the option of termination. I opted to wait for the test results, tests and results that would take a few more weeks.
From that moment of reading black text on a report, my whirlwind began.
I had evidently failed my baby, I couldn’t grow my baby right, it was surely my fault. Did I eat something wrong? Was it the electric blanket I used to warm the bed in winter? Was it the medication I took for nausea? I was now faced with this option – do I end my baby’s life or bring them into a world which sounded so hard for them. How do you make that decision? How do you make that decision when things are so uncertain?
I think there can be an assumption that prenatal diagnosis is about hearing about a condition and making a decision that feels right. But... what if there is no right. What if either pathway is potentially filled with pain? What if the diagnosis is uncertain and the outcomes are uncertain?
I wasn’t born with a congenital anomaly myself, and yet there were moments that I struggled so much. I recall days, weeks and months of not wanting to be here and yet in many ways I was privileged. What about my baby? What if they face all the hard things the literature said, all the hard things the doctors said. Would they be happy? Would they be abused in a society that treats disabled people differently? Would they fall through the gaps in life, like many people I met and tried to support as a health professional?
But, are society’s downfalls enough of a reason to end my baby’s life at 36 weeks pregnant? Am I strong enough? I would wonder what I would do with the things in the nursery if I ended my pregnancy then hate myself for thinking of such of materialistic stuff like that when there are much more important things to think about? Clearly, I thought, I’m just a horrible person.
The fetal MRI led to a change in Squishy’s diagnosis. A change that the obstetrician thought to mean slightly better odds than initially given. That was enough to try, that was enough to have some hope. I had somehow decided, as long as nothing else made things worse, I could continue, so I informed them that and left the clinic feeling like it marked the start of the next stage – I was committed and we were going to do this.
On the long drive home, I received a call from the same obstetrician, while she thought the odds were better, others in the team didn’t. They thought things were worse, they thought there was less hope. Prenatal diagnosis is far from this idea of just being told what can come and making a decision. It’s full of uncertainty. No matter what anomaly or condition, there is simply no way of foreseeing the future.
Gosh, I just wanted some certainty, at a time when Squishy was almost “term” and kicking up a storm, I was trying to cope with all these thoughts and feelings. I wanted to call the parenting line, but was I going to be a parent? It was all unknown again. Would they judge me? Would they try to convince me?
In the following weeks, care was transferred back to the country as I continued my pregnancy. I threw myself into trying to do things to help my Squishy, but standard healthcare had no answers for me other than my obstetrician appointments, so I turned to things I wouldn’t usually consider.
The natural medicine practitioner implied my piercing was responsible for my daughter’s anomaly and the person I saw for a pregnancy massage asked if my baby was going to be “enter slur”. I was alone when needing to answer the sonographer who asked me why I would continue my pregnancy as in her country, people terminate. It was hard to talk to people.
All these interactions just piled on, while I continued to see pregnant women everywhere. I struggled. I struggled for months after my baby was born, particularly the weeks while waiting to find out if she had a particular syndrome. She was perfect, I was not. I hid my struggle the best I could – I am a mental health professional, I chose this, I chose to continue the pregnancy so I felt like I couldn’t let anyone see how worried I was, that I wasn’t coping. I needed to keep my baby safe, her anomaly was rare, so I had to read everything to educate others, which also meant I worried about everything. I couldn’t sleep. I would triple-check, quadruple-check, just to try and get those intrusive images away. Many horrible images.
As a mental health professional, I knew I needed help. I referred myself to a psychologist who was lovely but acknowledged this was a new situation for her. It wasn’t a great fit because I felt like I wanted to find the joy or control but the focus was on loss.
I referred myself to early parenting supports, my baby struggled to feed and sleep, so it felt like we could get support from that angle without having to tell people my fears and how bad a parent I really was. I self-referred to a residential service, however, after going through the intake call, they simply said we weren’t eligible because of my daughter’s anomaly. It was hard. In my mind, that was to be my relief and it took so much to call, to go nowhere.
The months were so hard, with investigations for seizures, nasogastric feeds and trips to ED. I did meet kind and empathetic practitioners along the way, but it didn’t feel safe to talk about what was happening for me. Remember, I chose this when people told me it might be hard. I just tried to hide what was happening for me – so much I didn’t even tend to the ongoing consequences of my third-degree tear during labour.
I finally sought mental health support from a familiar practitioner, who was able to hold space and meet me where I was, which meant I was then able to be open with some of the thoughts, fears and self-blame and that was the start of feeling okay.
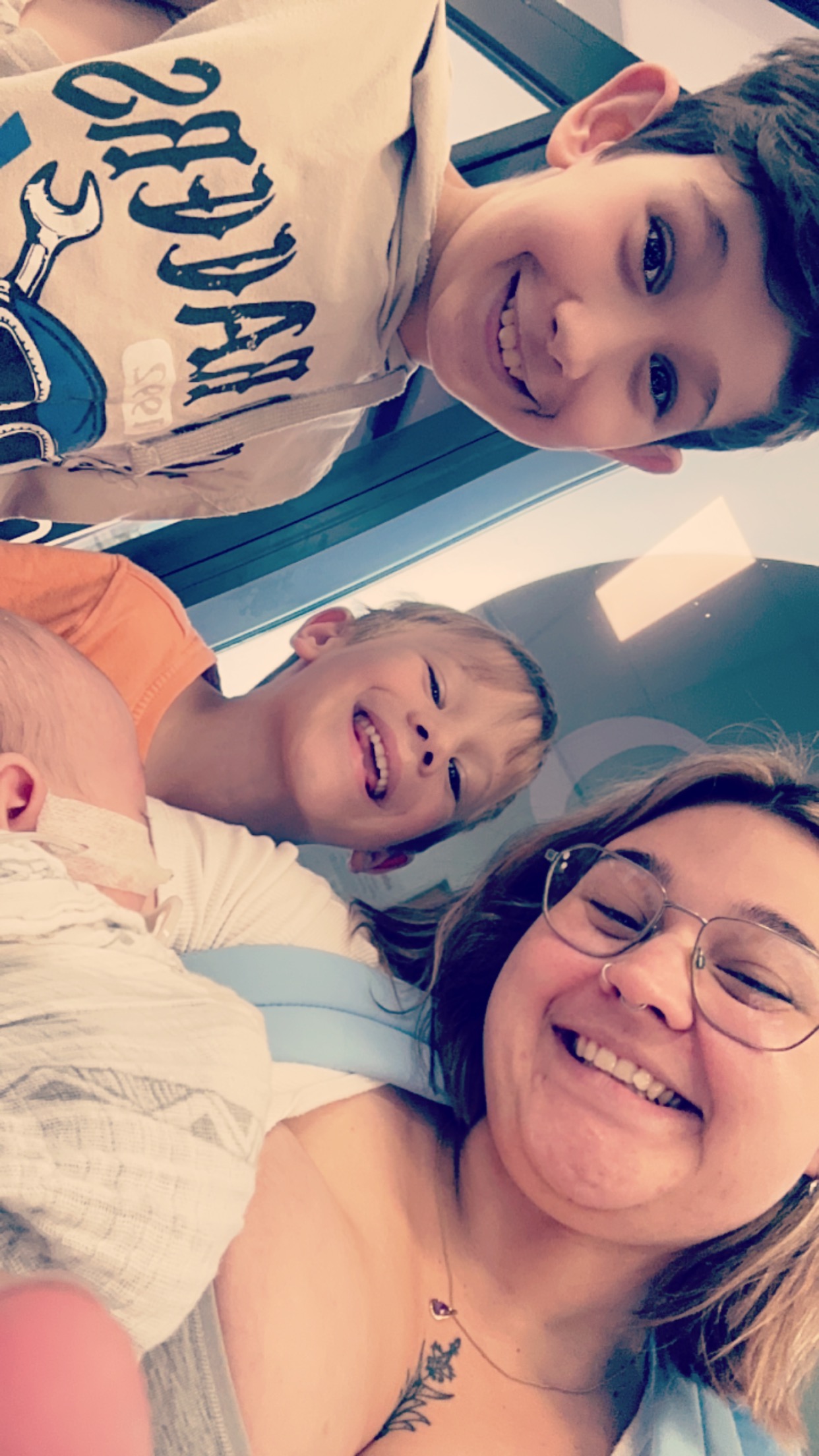
Pieta's Story
Please submit your details below and we will be in touch soon.
Related Fact Sheets























.png)

